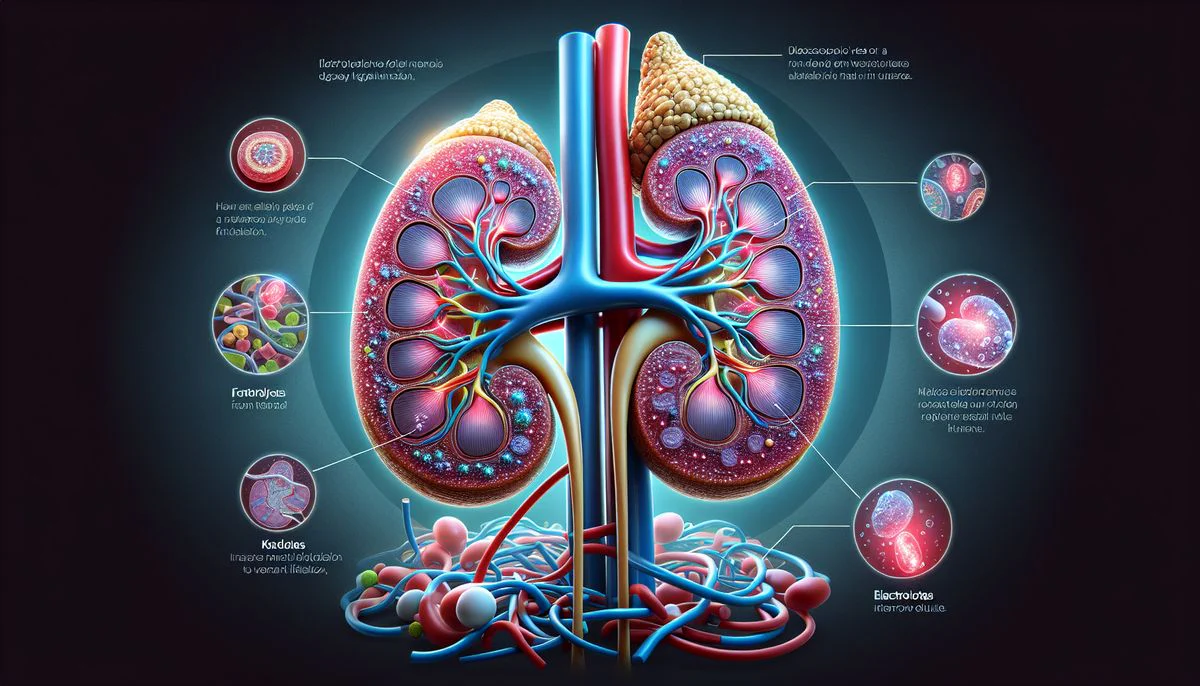
Electrolytes support the kidneys by helping regulate fluid movement, maintain electrical stability in cells, and guide essential filtration processes, and understanding how these minerals interact with kidney structures reveals why even small imbalances can disrupt overall health in noticeable and sometimes surprising ways.
Why do electrolytes play such an essential role in kidney function?
Electrolytes allow the kidneys to balance fluids while maintaining stable cellular activity. These minerals carry electrical charges that guide water movement. According to our editor’s research, kidneys rely on sodium, potassium, calcium, chloride, and magnesium to filter blood properly. Each electrolyte affects how fluid shifts across membranes. When levels drift too high or low, filtration becomes less efficient. This imbalance can affect blood pressure and urine output. Healthy electrolyte levels support smooth kidney work. Small shifts often produce big changes. This connection highlights why electrolytes deserve close attention.
How does sodium influence kidney filtration?
Sodium plays a major role in controlling fluid volume. The kidneys adjust sodium levels constantly. As a result of our editor’s reviews, sodium determines how much water the body retains. High sodium causes extra fluid retention. This increases the kidneys’ workload. Low sodium triggers fatigue and confusion because cells lose stability. Kidneys regulate sodium through reabsorption steps. These steps occur in different segments of the nephron. Proper sodium balance supports blood pressure control. It also helps the heart function smoothly. Understanding this link helps guide healthier choices.
Why does potassium matter for kidney and heart stability?
Potassium maintains electrical balance in tissues. The kidneys remove excess potassium carefully. According to our editor’s research, small increases in potassium can affect heartbeat rhythm. Kidneys filter potassium through multiple channels. When kidney function weakens, potassium may rise. This creates muscle weakness or irregular heartbeats. Low potassium also harms muscle function. Stable potassium levels support nerve communication. Good hydration helps regulate potassium excretion. Patients with kidney disease often receive potassium guidance. Careful monitoring protects heart safety.
How does calcium support kidney and bone health together?
Calcium affects muscle contraction, nerve activity, and bone strength. The kidneys activate vitamin D, which helps absorb calcium. As a result of our editor’s reviews, kidney dysfunction reduces vitamin D activation. This reduces calcium absorption from food. Low calcium may cause muscle cramps and bone weakness. The kidneys also remove excess calcium. High calcium can lead to stone formation. These stones create pain and infection risk. Balanced calcium supports long-term stability. Kidney and bone health remain closely connected.
Why does magnesium help stabilize cellular processes?
Magnesium supports hundreds of chemical reactions. Many enzymes require magnesium to function. According to our editor’s research, kidneys filter magnesium constantly. Low magnesium causes muscle twitching and fatigue. High magnesium appears in advanced kidney disease. This imbalance affects blood pressure and nerve activity. Magnesium interacts with calcium during muscle activity. Both minerals influence heart rhythm. Maintaining ideal levels protects cellular health. Diet often helps maintain magnesium balance. Regular monitoring becomes essential in kidney disorders.
How does chloride help maintain acid-base balance?
Chloride pairs with sodium to manage fluid movement. It also helps balance body pH. As a result of our editor’s reviews, chloride works with bicarbonate to manage acidity. Kidneys adjust chloride levels to stabilize pH after meals. Low chloride creates metabolic alkalosis. This condition reduces oxygen delivery. High chloride may cause fatigue or rapid breathing. Chloride remains essential for stomach acid production. Proper levels improve digestion. Kidney filtration keeps chloride within a safe range.
Why does the nephron depend so heavily on electrolyte movement?
The nephron uses electrolytes to filter and reabsorb fluids. Each nephron segment has a unique role. According to our editor’s research, electrolytes create concentration gradients that guide water movement. Sodium helps pull water out of the filtrate. Potassium handles electrical balance along tubules. Chloride stabilizes charge as molecules move. These gradients allow urine concentration to change based on body needs. Without electrolytes, filtration would collapse quickly. Nephron function depends entirely on this electrical and chemical precision.
How does hydration affect electrolyte balance and kidney work?
Hydration guides how electrolytes shift between blood and tissues. When dehydration occurs, electrolytes become concentrated. As a result of our editor’s reviews, dehydration forces kidneys to conserve water. This increases sodium levels and causes fatigue. Overhydration dilutes electrolytes too much. Low sodium becomes dangerous in these cases. Balanced hydration supports stable kidney function. Proper water intake allows electrolytes to move smoothly. This balance prevents strain on filtration pathways. Hydration habits influence overall wellness significantly.
Why do certain medications alter electrolyte levels?
Medication affects kidneys by changing filtration or altering electrolyte exchange. Diuretics remove fluid by adjusting sodium and potassium levels. According to our editor’s research, some blood pressure medications increase potassium retention. Other medications increase calcium loss. Patients taking certain treatments require frequent testing. Medication effects vary widely among individuals. Kidney specialists adjust doses to avoid dangerous shifts. Understanding medication impact creates safer treatment results.
How does kidney disease disrupt electrolyte stability?
Kidney disease reduces the ability to filter waste and balance minerals. Potassium may rise quickly. Sodium may fall with fluid retention. As a result of our editor’s reviews, acid levels increase when kidneys cannot remove hydrogen ions. These shifts create fatigue, confusion, and muscle weakness. Early kidney disease shows mild imbalances. Advanced stages produce dramatic changes. Treatment focuses on stabilizing electrolytes. Dietary adjustments reduce complications. Regular monitoring prevents emergencies.
Why do dietary choices matter so much for electrolyte control?
Food provides major sources of electrolytes. Salty foods increase sodium intake. Fruits provide potassium. Dairy offers calcium. According to our editor’s research, balanced meals prevent overload. Kidney patients receive custom diet plans to control mineral intake. Hydration also supports dietary balance. Lifestyle choices influence kidney workload daily. Small adjustments create long-term benefits. Dietary awareness reduces disease risk.
How do specialists monitor electrolytes during kidney treatment?
Specialists use blood tests to measure mineral levels. Testing identifies early changes. As a result of our editor’s reviews, regular monitoring tracks treatment progress. These tests help adjust medications and diet. Urine tests confirm kidney response. Specialists watch for patterns over time. Monitoring provides peace of mind. It also prevents complications. Each test supports personalized care. Consistent checkups protect kidney health.
